
| Centre Name: | 
Centre for Research on Communicable Diseases (CRCD) (https://crcd.research.utar.edu.my/) |
| Chairperson: | Prof. Dr. Ngeow Yun Fong |
| Description of Centre: | Communicable diseases, defined as bacterial, viral, fungal and parasitic infections that can be transmitted to humans via the environment, animals and other human beings, continue to be a major health problem in many parts of the world. In Malaysia, infections still rank third as a cause of morbidity and mortality among patients admitted to public and private hospitals (MOH health facts, 2016). Climate change, political turmoil and misuse of antibiotics have all been blamed for the increasing health burden from infections. With global travel of humans, animals and disease vectors, comes the global transmission of diseases. Hence, Malaysia, being a meeting point of global communities, can no longer afford to focus only on the control of traditional tropical diseases. We have to be alert to the possibility of importation of new infections and to be equipped with the knowledge and resources to prevent their dissemination in our country.
While many infections are preventable with vaccination, the use of anti-infective agents and hygienic practices, new infections are continuously emerging as a result of microbial evolution, selection by human interference and geopolitical changes. In recent decades, epidemics such as SARS, MERS, Nipah, Zika and avian/swine influenza have taken a heavy toll on human health. More critically, the emergence and dissemination of multidrug-resistant bacteria is threatening the end of modern medicine, as the lack of effective treatment for infections is making interventions such as joint replacement, organ transplantation and cancer chemotherapy almost too dangerous to undertake. The World Health Organization has declared antibiotic resistance as a global crisis (WHO 2015). There is obviously, an urgent need for health care systems, world-wide, to respond to such threats. University research centres can contribute significantly towards the prevention and control of infections. Research findings can lead to new products and interventions or the more effective use of existing products and interventions. A better understanding of causes and consequences of infections and the link between infectious and non-infectious diseases, for instance, the association between diabetes and TB, is crucial for effective targeted interventions and management strategies. An indispensable tool in infection research is surveillance, to understand patterns of disease emergence, to map, monitor and evaluate trends, and to measure the effectiveness of disease control programmes. Currently, data is still lacking for many infectious diseases. Innovations and novel approaches are required to enable improved surveillance coverage, particularly in resource poor areas. |
| Research area: |
The CRCD will support research (both basic and applied) on all communicable diseases, particularly the infections that are prevalent and important in Malaysia and SE Asia. The following are examples:
Other research areas to be encouraged include: |
| No. | Name | Faculty | Member |
|---|---|---|---|
| 1 | Senior Professor Dr Ngeow Yun Fong | FMHS | Chairperson |
| 2 | Dr Wong Jun Leong | FMHS | Secretary |
| 3 | Dr Aw Kar Men | FMHS | Assistant Secretary |
| 4 | Senior Professor Dr Yap Sook Fan | FMHS | Member |
| 5 | Clinical Senior Professor Dr Jenny Parameshvara Deva @ nee Ng Gek Pheng | FMHS | Member |
| 6 | Professor Dato' Dr Lye Munn Sann | FMHS | Member |
| 7 | Associate Professor Dr Gan Seng Chiew | FMHS | Member |
| 8 | Clinical Associate Professor Dr Naghem Farouk Abed Abed | FMHS | Member |
| 9 | Clinical Associate Professor Dr Thaw Zin | FMHS | Member |
| 10 | Assistant Professor Dr Chuah Candy | FMHS | Member |
| 11 | Assistant Professor Dr Ong Hooi Tin | FMHS | Member |
| 12 | Assistant Professor Dr Saw Seow Hoon | FSc | Member |
| 13 | Assistant Professor Dr Shwe Sin | FMHS | Member |
| 14 | Clinical Assistant Professor Dr Divyangana Kiran Vartak | FMHS | Member |
| 15 | Clinical Assistant Professor Dr Kye Mon Min Swe | FMHS | Member |
| 16 | Clinical Assistant Professor Dr Lin Phyo Phyo San | FMHS | Member |
| 17 | Clinical Assistant Professor Dr Zay Yar Naing | FMHS | Member |
| 18 | Dr Hnin Pwint Phyu | FMHS | Member |
| 19 | Ts Ms Saw Seow Hui | FSc | Member |
| 20 | Dr Lee Kai Wei | FMHS | Associate Member |
| 21 | Dr Ng Hien Fuh | FMHS | Associate Member |
| 22 | Dr Nic Musa Kek bin Abdullah | FMHS | Associate Member |
| 23 | Dr Wang Xueling | FMHS | Associate Member |
| 24 | Madam Sargit Kaur A/P Chanan Singh | FMHS | Associate Member |
| 25 | Mr Chay Min Jie | FMHS | Associate Member |
| 26 | Mr Zain Illyaaseen Bin Kairudin | FMHS | Associate Member |
| 27 | Ms Dawn Carmel Paul | FMHS | Associate Member |
| 28 | Ms Jamie Ng May Ling | FMHS | Associate Member |
| 29 | Ms Lee Col Lin | FMHS | Associate Member |
| 30 | Ms Mahfuzah bt Mohamad Azranyi | FMHS | Associate Member |
| No. | Date | Event |
|---|---|---|
| 1 | 21 February 2020 | Health Talk on “Degradation of Maternal Antibodies in Infants” |
| 2 | 12 June 2020 | Webinar Covid 19 The Virus and The Host |
| 3 | 15 September 2020 | Hepatitis C: The Journey from Discovery to A Cure |
| 4 | 23 – 27 November 2020 | UTAR COVID-19 AWARENESS WEEK 2020 (UCO19AW20) |
| No. | Date | |
|---|---|---|
| 1 | Health Talk on “Degradation of Maternal Antibodies in Infants”
Measles is a serious disease that can cost millions of life from an outbreak and it is easily spread through coughs and sneezes from the infected people. Major epidemics usually occur approximately every two to three years and it would bring an estimated 2.6 million deaths each year. With the discovery of vaccine in 1963, the fatal counts had reduced tremendously until today. However, the number is yet to be proud of as the World Health Organization (WHO) reported that more than 140,000 people died from measles in 2018 with mostly children under the age of five years old. With vaccination for measles accessible worldwide, the next question in line is how early should a person receive artificial immunity. To address this issue University of Michigan School of Public Health Research Assistant Professor Dr Abram Wagner shared his study conducted with 891 pairs of infant and mother in Tianjin, China and 400 pairs in Chandigarh, India. Dr Wagner was in UTAR Sungai Long Campus to share his study findings on the degradation of maternal antibodies in infants on 21 February 2020. “An infant is not vaccinated at birth because they have maternal antibodies to protect them,” said Dr Wagner. With different regulations in different countries, the earliest measles vaccination given to an infant is at six months old. The reason it is not given too early may also be due to the possibility that babies may not respond well to the vaccinations. The concern, however, was raised through the study conducted in Chandigarh where less than half of the 400 pair of participants were still protected by the maternal immunity after three months. In other words, there are a few months where the infants will be left unprotected until they receive their first vaccination. As a way to overcome this, Dr Wagner suggested an early measles vaccination at four months old, without replacing the vaccination that will be received later on at nine or twelve months old. Despite being a possible solution, the idea came with its own drawbacks. Adding another vaccination in the existing schedule would mean additional cost, and it can be a significant amount especially to developing countries. “Perhaps the mother can be vaccinated more but we still do not know if it will increase the immunity in the baby,” said Dr Wagner. |
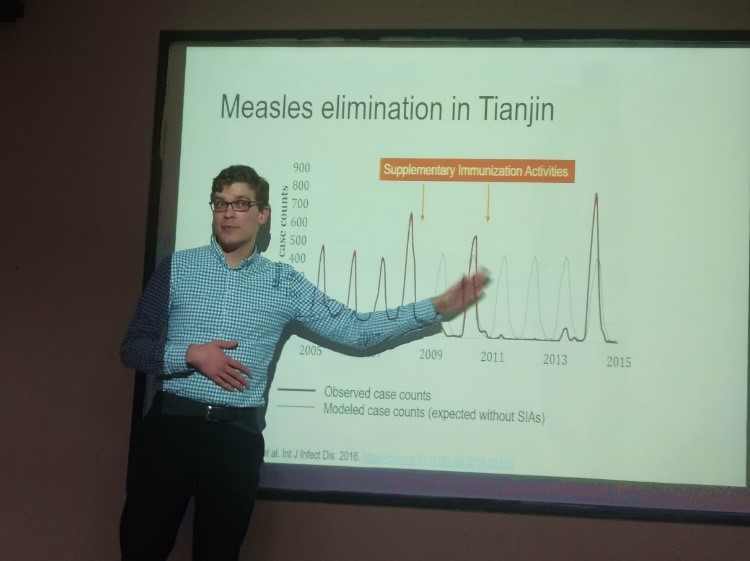
Dr Wagner during the talk 
Faculty of Medicine and Health Sciences Clinical Assoc Prof Dr Myo Oo (right) presenting a token of appreciation to Dr Wagner |
| 2 | Webinar Covid 19 The Virus and The Host
https://www.youtube.com/watch?v=w9uN9moV1eA |
|
| 3 | Hepatitis C: The Journey from Discovery to A Cure
UTAR Centre for Research on Communicable Diseases (CRCD), in collaboration with Department of Soft Skills Competency (DSSC) of Sungai Long Campus, organised a physical and virtual talk titled “Hepatitis C: The Journey from Discovery to a Cure” on 15 September 2020. The event saw the attendance of about 140 participants. Invited to deliver the talk was Dr Chung Yun Chien, a Consultant Hepatologist and Gastroenterologist at Hospital Selayang. In his talk, Dr Chung first provided a general idea on Hepatitis C (HCV). “Hepatitis C Virus is essentially an RNA virus. There are five main types of hepatitis viruses, namely A, B, C, D and E. All the hepatitis diseases are RNA viruses except Hepatitis B, which is a DNA virus. There are other types of RNA virus of Flavivirus such as Dengue, Yellow Fever and Zika Virus. No vaccine is currently available to prevent Hepatitis C, but there is a vaccine for Hepatitis B. It is actually similar to the dengue virus. To date, there is no vaccine to prevent the complication and development of dengue virus,” he said. He added that the issue with the Hepatitis C virus is the heterogeneity of the virus itself, which allows the virus to escape from the host immune system and medications as well as vaccines. He presented the worldwide distribution of HCV genotypes, saying that HCV genotype three (54.5 per cent) was the most prevalent genotype in Malaysia, followed by genotype one (40 per cent). He also explained what would happen if an individual was exposed to HCV and he pointed out its difference with Hepatitis B (HBV). “Between 2003 and 2017, only about 23,000 Hepatitis C had been notified to the MOH. This is just the tip of the iceberg. There are a lot of people walking around with Hepatitis C without knowing it. It was reported that the incidence of Hepatitis C had increased from 2.65 per 100,000 populations in 2015. Regardless of males or females, slightly more than 50 per cent of the patients were in the younger age group that is between 26 and 45 years old. Most of the reported patients were of Malay ethnicity,” said Dr Chung. He stressed that the figure presented was dependent on how the case was reported. He also demonstrated the projection of the current and future disease burden of HCV infection in Malaysia and explained the exposure known to be associated with HCV infection such as injecting drug use and sharing needles, blood transfusions before the year 1994 (transplanted from an infected donor), occupational exposure to blood, birth to an HCV-infected mother, and sex with an infected partner. Furthermore, he explained how to determine an individual who has been infected with the HCV virus and who should be screened for HCV. “Hepatitis C can be cured. Treatment should be given to every individual regardless of who they are, where they come from, and the status of their liver disease,” he said. Dr Chung moved on to a more positive note, in which he spoke about the treatment of HCV, which was the most important part of the talk. He stated that the primary goal of therapy would be to cure HCV for everyone infected. “Those cured of HCV would have their blood show a sustained virologic response (SVG), after 12 weeks of treatment. The cured patients tend to have reduced liver inflammation, improvements in extrahepatic manifestation and liver necroinflammation, regression of hepatic fibrosis and reduced risk of liver cancer, or Hepatocellular Carcinoma (HCC),” said Dr Chung. He also reminded the participants that while everyone with HCV should be treated, there are three categories of people that need to receive prioritised treatment to prevent the spread of the disease. Speaking on this, he added, “There are the highest priority patients, which consist of those in need of an organ transplant, who have advanced fibrosis (F3 to F4) and extra-hepatic manifestations. Then comes the high priority patients, which are patients with fibrosis 2 or more, co-infected with Hepatitis B (HBV) or HIV or with other chronic lung diseases (CLD). Lastly, there are those that have an increased risk of transmission, such as healthcare workers, incarcerated people and patients on hemodialysis.” Dr Chung then described the HCV pre-treatment assessment or the assessment of liver fibrosis in patients. He pointed out several techniques to evaluate the prevalence of liver fibrosis; “There is the normal liver ultrasound method and also the liver transient elastography or also known as fibroscan, which is a non-invasive technique that uses both ultrasound and low-frequency elastic waves to quantify liver fibrosis. There is another method called the liver biopsy; this, however, is less often used because it has a high mortality rate,” said Dr Chung. Afterwards, he shared a roadmap of the progress that the medical world has made, in terms of finding a cure for HCV. A noteworthy milestone that he pointed out was during the 2000s, where Pegylated Interferon (PEG-IFN) and Ribavirin were introduced, increasing the cure rate to almost 60 per cent. Similarly, in 2011, the first antivirals, Boceprevir & Telaprevir were combined with PEG-IFN and Ribavirin and it subsequently improved the cure rate to 70 per cent. However, all these medications were ceased after a while, due to the horrible side effects. From there, he spoke on several other important topics, such as the HCV replication cycle and drug targets in Chronic Hepatitis C (CHC), the potential mechanism of action of Ribavirin in CHC treatment, Direct Acting Antivirals (DAAs) and Europe approved and recommended HCV DAAs. Dr Chung concluded the talk with a few key messages, whereby he mentioned that screening of high-risk individuals is very important and a cure is possible. |

Dr Chung delivering his talk 
An enlightening Q&A session with Dr Chung 
CRCD Chairperson Prof Dr Ngeow Yun Fong (right) presenting a token of appreciation to Dr Chung |
| 4 | UTAR COVID-19 AWARENESS WEEK 2020 (UCO19AW20)
OBJECTIVES: UTAR COVID-19 Awareness Week 2020 (UCO19AW20) aims to increase awareness of the global pandemic and to encourage best practices among the general public, academic staff, non-academic staff and all students in UTAR to avoid the further emergence and spread of COVID-19. UCO19AW20 is all about sharing the right information on what we can all do to help halt the spread of infection, including understanding the COVID-19 virus, how the disease started and how it spreads. In addition, the strategies used by scientists around the globe to combat the virus will be presented by UTAR students. THEME: STAY ALERT, STAY CALM, STAY SAFE (S3ACS)! |
|